A first for ophthalmology: FOR 2240 team wins Erwin Niehaus Prize
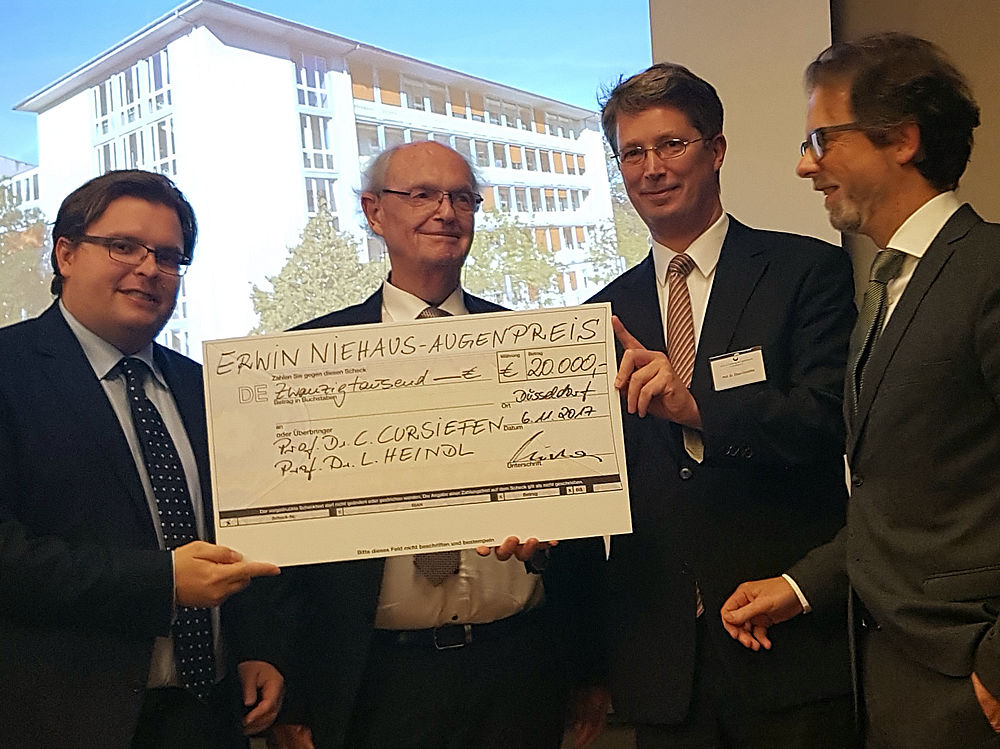
On November 6th, 2017, the prestigious Erwin Niehaus Prize was awarded to the Department of Ophthalmology (Cologne) in the Industry Club in neighboring Duesseldorf, and it was the first time this prize was awarded to ophthalmologists. Prof. Claus Cursiefen, who is Chair and Professor at the Dept. of Ophthalmology and Speaker of the DFG Research Unit FOR 2240, and Prof. Ludwig M. Heindl, who is the leader of the ophthalmo-oncology group in Cologne and Principal Investigator of Project 4 in the FOR 2240, were recognized for their work on the topic of “Split-cornea transplantation: sharing helps seeing.”
Normally, the cornea is transparent, and to a certain extent it can be thought of as the “windshield” of the eye. If the cornea becomes less transparent, this results in vision becoming worse or even lost. Loss of corneal transparency is the second most common cause of blindness worldwide. Typically, corneal transplantation is the standard therapy. As in all branches of transplantation medicine, there is a grave shortage of donor tissue, and this leads to long waiting periods and avoidable blindness.
In several highly ranked publications, Prof. Cursiefen and Prof. Heindl demonstrated that instead of using one donor cornea for one recipient, as is usually done, a new, minimally invasive surgical technique allows one donor cornea to be used for two or more patients.
They achieve this dual or multiple usage with a new lamellar surgical technique. This minimally invasive technique allows just the diseased part of the cornea to be removed and exchanged for the corresponding healthy part of the donor cornea. Thus, it is no longer the case that the entire cornea is removed and replaced. Since 2011, minimally invasive lamellar transplantation techniques like DMEK and DALK have increasingly replaced penetrating keratoplasty. Next to a faster and better recovery of visual acuity, the main advantage of the lamellar techniques is that they are much safer. A study of 1000 DMEKs performed at the University Hospital of Cologne with at least one year of follow-up showed that the rate of rejection was only two percent.
When an operation using the technique known as “DALK” is performed, clouding of the frontal part of the cornea, as is typically found with keratoconus, is treated by replacing the frontal 98 percent of the corneal tissue. When an operation using the technique known as “DMEK” is performed, only the very thin endothelial layer of the cornea is selectively replaced when it is only this very thin endothelial layer that is diseased.
What this allows for is just one donor cornea to be used for more than one patient: one who is having a DMEK and one who is having a DALK. Thus, many more patients can be provided with donor tissue and regain their ability to see well through the use of these procedures at the Department of Ophthalmology at the University Hospital of Cologne. The University Eye Hospital of Cologne is a leading one in Europe for modern, minimally invasive corneal transplantation surgeries. With over 600 transplantation performed in a year, it is here that more than 10% of all corneal transplantation are performed in all of Germany.
[This post is based on the German-language article https://augenklinik.uk-koeln.de/informationen/aktuelles/detailansicht/teilen-hilft-sehen-preis-fuer-minimalinvasive-hornhauttransplantationschirurgie/ published 09.11.2017].